
Such ventilatory settings usually lead to high inspiratory pressures and overdistention of the alveolar unit. Historically, large tidal volumes were the approach in patients requiring mechanical ventilation to minimize atelectasis and improve oxygenation and ventilation. Most of the mechanisms have their basis in overdistention and increased pressures in the alveoli. Researchers have described several mechanisms in the literature for the rupture of alveoli. The exact pathophysiology for lung injury and barotrauma due to mechanical ventilation remains unclear however, evidence suggests that overdistention and increased pressures in the alveoli units lead to inflammatory changes and possibly rupture and leakage of air into the extra alveolar tissue. If higher PEEP is necessary for oxygenation, it should be titrated up slowly with close monitoring of the peak inspiratory and plateau pressures.
However, clinical data has not associated increased PEEP with increased risk of barotrauma when used in conjunction with lung protective strategies, such as low tidal volume and target plateau pressure under 30 cmH2O. Įlevated positive end-expiratory pressure (PEEP) may theoretically lead to overdistention of healthy alveoli in regions not affected by disease and ultimately barotrauma. The risk for barotrauma increases whenever the peak pressures and plateau pressures become elevated to the same degree. Peak pressure is the plateau pressure in addition to the pressure needed to overcome flow resistance and the elastic recoil of the lungs and chest wall. Based on current data, as well as the increased mortality associated with barotrauma, the ARDSnet protocol suggests keeping plateau pressures below 30 cmH2O in patients on mechanical ventilation for ARDS management.

Plateau pressures are easily measurable on a ventilator by performing an inspiratory hold. Elevated plateau pressures, particularly pressures higher than 35 cmH2O, have been associated with an elevated risk for barotrauma.

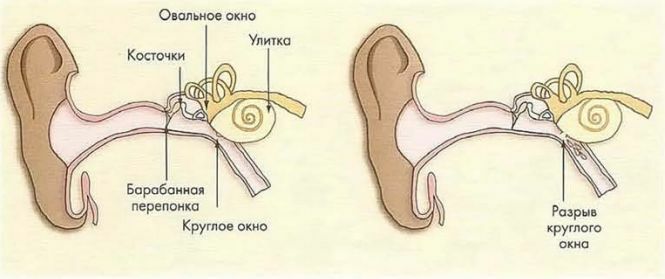
Plateau pressure is the pressure applied to the alveoli and other small airways during ventilation. Įlevated plateau pressure is perhaps one of the most critical measurements of which to be aware. In many instances, auto-PEEP may lead to ventilator asynchrony, increased alveoli distention, and ultimately barotrauma. When intrinsic PEEP is present, it imposes an additional force that the inspiratory muscles have to overcome to trigger a breath. In many cases, auto-PEEP results in ventilator asynchrony, which may result in an increased risk of barotrauma. For a patient to be able to trigger a breath on the ventilator and for the flow to begin, the inspiratory muscles must overcome the recoil pressure. The static auto-peep is easily measurable on a ventilator by performing an expiratory pause by using this method you would obtain the total PEEP, the external PEEP subtracted from the total PEEP will equal the intrinsic PEEP or auto-PEEP. Dynamic hyperinflation can be managed by decreasing the respiratory rate, decreasing the tidal volume, prolonging the expiratory time, and in some cases by increasing the external PEEP on the ventilator. It leads to overdistention of the alveoli and increases the risk for barotrauma. The hyperinflation is progressive and worsens with each tidal volume delivered. As a result, there is an increase in the intrinsic positive end-expiratory pressure (PEEP), also known as auto-PEEP.
#TREATMENT FOR PULMONARY BAROTRAUMA FULL#
These patients have a prolonged expiratory phase, and therefore have difficulty exhaling the full volume before the ventilator delivers the next breath. Patients with obstructive lung disease, COPD, and asthma are at risk of dynamic hyperinflation. These diseases are associated with either dynamic hyperinflation or poor lung compliance, both of which predispose patients to increased alveolar pressure and ultimately barotrauma. Specific disease processes, including chronic obstructive pulmonary disease (COPD), asthma, interstitial lung disease (ILD), pneumocystis jiroveci pneumonia, and acute respiratory distress syndrome (ARDS), may predispose individuals to pulmonary barotrauma. When managing a ventilator, physicians and other health care professionals must be aware of these risks to avoid barotrauma. However, certain ventilator settings, as well as specific disease processes, may increase the risk of barotrauma significantly. Elevation in the trans-alveolar pressure may lead to alveolar rupture, which results in leakage of air into the extra-alveolar tissue.Įvery patient on positive pressure ventilation is at risk of developing pulmonary barotrauma. Positive pressure ventilation may lead to elevation of the trans-alveolar pressure or the difference in pressure between the alveolar pressure and the pressure in the interstitial space. Pulmonary barotrauma results from positive pressure mechanical ventilation.


 0 kommentar(er)
0 kommentar(er)
